The evolution of electrocardiogram (ECG) technology has contributed to our understanding of cardiac physiology, the role of electricity in sustaining human life, and how to interpret the signals broadcast by our bodies. Increasingly, it’s allowing us to gain a more comprehensive and easily accessible picture of our overall health.
The early days of electrocardiogram technology involved expensive and experimental medical equipment limited to a handful of labs and hospitals. Today, ECG tech can be found in wearable consumer items weighing no more than a few grams. Understanding the function and progression of ECG technology helps us predict where the technology will go—and reveal what is already possible.
What is ECG?
ECG stands for electrocardiogram, traditionally a test which is done to assess the muscular and electrical functions of the heart. Most people associate ECG monitoring with a line tracing on a piece of paper, or a digital display of the heart’s electrical and muscular activity—the heartbeat.
An electrocardiogram records the electric impulses which originate in and travel through your heart. The electric impulse originates ECG is incredibly important for exploring the causes of a variety of cardiac problems, including heart attack, angina, and palpitations.
Don’t You Mean EKG?
ECG and EKG both stand for the same thing—EKG is an abbreviation from the German “Elektro-kardiographie”. It is still, however, commonly used in non-German-speaking countries. Either abbreviation is correct.
Regardless of how you choose to spell it, when ECG / EKG data is collected via biosensor and interpreted using digital algorithms, it can create a picture of the following advanced biometrics of the user, including:
- Heart Rate
- Heart Rate Variability
- Stress
- Fatigue
- Heart Age
- Breathing Index
- Mood
How Does ECG Work?
To understand how ECG works, you must first understand how the human heart works. The heart has four main chambers—the left and right atria, and the left and right ventricles.
Each heartbeat is triggered by the depolarization (a dramatic electrical change) of the sinoatrial node, located in the right atrium. The electric signal travels along specialized heart muscle cells called purkinje fibers, and triggers the associated muscular contraction of the atria. This causes an increase in pressure within the atrial chambers, forcing blood into the ventricles. Blood then leaves the ventricles and travels to other parts of the body.
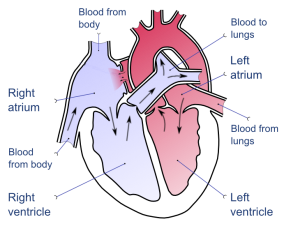
When you listen to a heartbeat, what you’re hearing is the valves closing between the atria and the ventricles, ensuring that blood flow only occurs in one direction and not back into the atria. The musculature response of the heart to an electric “prompt” is audible with the use of a stethoscope. The electric trigger is, obviously, not audible—but it can still be recorded via ECG.
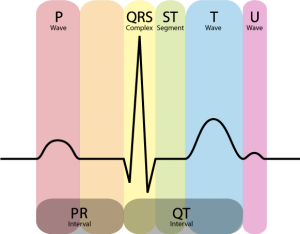
The ECG measures the electrical activity of the heart over time. First, a small current indicates the depolarization of the sinoatrial node. Then, the current travels via the purkinje fibers to the node between the atria and the ventricles. Finally, the ventricles depolarize. In a healthy heart, this series of events happens with predictable regularity and at consistent intervals. Any irregularities in the sequence—for example, too much time between depolarization of the atria and the ventricles, respectively—can tell the observer much about the function of the heart being monitored by ECG.
History of ECG
The development of ECG technology began in the 19th century, and helped shape our understanding of the function of the human heart. Interestingly, recent developments in ECG technology mirror those early experiments—before researchers even perfected the recording of the electrical signature of the heart, they were looking for innovative ways to transmit the data.
Dutch physiologist Willem Einthoven recorded a human ECG in March 1905 and transmitted it from the hospital to his lab over a kilometre away—the first “telecardiogram”. Einthoven would later win the Nobel prize for inventing the electrocardiograph.
In 1949, the first truly mobile ECG device was developed by American physician Norman Jeff Holter. The Holter Monitor, a backpack which could record the ECG of its wearer and transmit the signal, weighed a whopping 75 pounds in its first incarnation.
Alongside the development of this technology, researchers and physicians were discovering how ECG technology could help them treat and cure patients. The varying electric signatures of the heart were interpreted and studied, leading to better understanding and treatment of cardiac problems such as angina and atrial arrythmia. This research led directly to the invention of the defibrillator, saving countless lives since its creation.
In 1978, Dr. Michael Mirowski et al. filed a US patent for a transistor circuit which analyzed ECG signals and could detect abnormal changes in heart rhythm. This was the first practical application of ECG technology in which the data output was interpreted by a computer algorithm rather than a human.
In 1999, Texan researchers demonstrated that wireless ECG technology transmitting data to hand-held devices was feasible and, more importantly, could be reliably interpreted by cardiologists.
Since then, wireless ECG technology has continued to evolve, bringing NeuroSky to where we are today—pioneers on the forefront of wireless and wearable ECG technology for device and electronics manufacturers and consumers.
ECG Biosensors and Applications
We’ve come a long way since the 75lb Holter Monitor. Now, virtually weightless chips just millimetres wide—like the NeuroSky CardioChip™ ECG biosensor, which is the world’s smallest at just 3mmx3mm—can transmit wireless data about the wearer’s cardiac cycle. Advances in mobile signal-processing and semiconductor technologies capture bio-signals in ways previously thought to be impossible.

Gone are the days when interpreting ECG data required a team of cardiologists. Sophisticated biometric algorithms can capture, analyze, and share valuable metrics pertaining to heart function and overall wellness.
As consumer interests continue to trend toward monitoring and improving overall health, modern ECG technologies play a critical role in the development of high-demand mobile health devices. You’d be hard-pressed to find a consumer even among the most health-conscious demographics willing to wear a Holter Monitor on their daily run, but the significant processing capability and complementary digital tracking services of today’s wearables fit in sleek, discreet, and fashionable wearables.
Consider the ever-increasing popularity of fitness tracking wristbands, measuring heart rate variability (HRV) to track individuals’ improvements in regular aerobic activity, and reliably calculate daily energy expenditures. HRV can also be used to monitor and interpret other important and interesting health metrics like mood, stress level, fatigue, recovery from strenuous exercise, and more.
Using ECG Biometrics
Not too long ago, ECG electrical biosensors could only be found in expensive medical equipment. Now, not only are they small enough to enable consumer wearable and mobile devices, but the development of biometric algorithms to translate ECG data allows the average person to see and understand their individual health metrics.
Another type of biosensor is also in commercial use. Photoplethysmography (PPG) technology delivers similar results to ECG biosensors, but with a few limitations. PPG senses the body’s rate of blood flow using a light-based technology. It works on the principle that hemoglobin absorbs light both in transmission and in reflectance mode. Measuring reflected light from the skin allows PPG to gauge the change in blood flow in each cardiac cycle.
While PPG has been a popular choice for some wearable technologies—likely due to its lower manufacturing cost—it does not always provide reliable data. Challenges with PPG include cancelling the effects of ambient light and accommodating differences in skin color and condition. PPG works best on parts of the body that have a high concentration of blood vessels, so it can be difficult to get reliable signals from the wrist using PPG.
In contrast, ECG biosensors like the NeuroSky BMD101 are capable of delivering a wide range of health metrics by capturing more comprehensive signals of overall heart performance from many areas of the body.
Collecting accurate health metrics is only one half of the equation. The end user must be able to interpret those metrics and be provided with actionable information. Most purchasers of consumer mobile health devices aren’t trained cardiologists—so complex biometric algorithms are required to provide context around the data.
Why Track Biometrics with ECG?
Once ECG data is collected and interpreted with accompanying algorithms, it can provide valuable and actionable insight to the user’s overall health. ECG data can shed light on the following health concerns:
Stress
Stress is the human body’s natural response to changing conditions. Like an alarm system, it’s hard-wired to protect us against threats, real or perceived. The physical response associated with stress involves a surge of hormones which increase heart rate, elevate blood pressure, and boost short-term energy supplies to power the fight-or-flight response.
While a moderate amount of stress on the body is normal, extended periods of high stress can contribute to a number of health problems concerning the digestive and immune systems. Long-term stress can also disrupt parts of the brain which regulate mood and motivation.
By learning to identify which types of events or situations trigger stress, individuals who monitor their stress levels via ECG-enabled wearables can take the steps necessary to help them live healthier and longer lives.
Mood
Like stress, situations resulting in both positive and negative moods can result in changes in bodily function. As explored in a Harvard Health article, a negative mood can directly impact the cardiovascular system by releasing stress hormones which cause heart rates to increase. This kind of emergency response can be chronic in individuals who are depressed or anxious, causing long-term heart responsiveness issues. Additionally, A 2007 Norwegian study found that participants with major symptoms of depression had a higher risk of death from causes including heart disease, respiratory illnesses, stroke, and more.
Wearable and mobile devices powered by ECG biosensors and algorithms can help users monitor their moods—identifying negative triggers, and empowering them to make changes to improve their lives.
Recovery
Intense exercise or exertion causes changes in the body such as breakdown of muscle tissue. The body must recover from this kind of exertion, and it’s a team effort—chemical and hormonal balance, the nervous system, and mental state must be restored along with any damaged tissues.
Serious athletes know that recovery is a critical part of any sports training program, and is necessary to ensure good future performance. Neglecting to build recovery time into a training program can result in general illness, mental health issues including depression, increased risk of injury, and other performance problems.
Even people participating in moderate intensity training programs need to factor in recovery time to their schedules. ECG biosensors and algorithms can assist in improving the recovery process, allowing people to plan their training sessions much more effectively.
Fatigue
Fatigue isn’t just “feeling tired”—it’s characterized by a feeling of lethargy or lack of energy that doesn’t go away after a period of rest. You can feel fatigued both physically and mentally (and, often, both at the same time).
Fatigue can be caused by chronic lack of sleep, poor nutrition, or excessive exertion. Sometimes, it can be caused by stress, anxiety, depression, grief, or an underlying medical problem requiring additional treatment.
HRV readings from ECG biosensors can help track habits which may lead to fatigue, cluing users in to triggers of their fatigue or ruling out more obvious causes of fatigue.
ECG Tech and Device Manufacturing
Manufacturing ECG-enabled devices necessitates using incredibly precise equipment which is also practical for use in wearables—meaning it has to be small. One advantage of NeuroSky’s BMD101 electrical biosensor is its integration of all the functional blocks required for ECG signal processing. The inclusion of a voltage regulator and RC oscillator on a single chip means no external devices or components are required. Small footprint wearable devices are made possible—and incredibly accurate—with this kind of ECG electrical biosensor.
The rapidly evolving landscape of mobile health devices and electronics means ODMs and OEMs must be able to develop innovative mobile health solutions and bring them to market quickly. Integrated biosensors enable this process for a wide range of device types and applications.
Additionally, ECG-based solutions allow HRV data to be accurately measured as peak intervals (the peak of each wave on a traditional ECG test) can be extracted with millisecond-level accuracy. Meaningful HRV data can be obtained even with short-duration measurements. Since ECG technology directly uses the electrical signals associated with heart activity, its accuracy is unparalleled.
A market-ready ECG biosensor will have a built-in software development kit allowing for easy app development for the most commonly used mobile platforms—namely, Android and iOS. The fewer barriers between an innovative mobile health application and the consumer market, the more likely it is to be a success.
Some exciting new applications of ECG biosensor technology involve stress and mood monitoring. Heart rate monitors have become relatively commonplace (although innovative new applications of HRV monitoring tech are still coming to market, including more specialized devices made for more advanced fitness enthusiasts who do intense interval training), but the health-conscious consumer may find monitoring these other wellness metrics appealing. NeuroSky’s Stress Index algorithm uses clinically proven derivatives of HRV to calculate stress which, beyond its immediate effects, has been shown to be an excellent predictor of future health problems.
NeuroSky’s ECG CardioChip™
The NeuroSky CardioChip™ ECG biosensor enables truly accurate and highly wearable mobile health solutions which can make a significant difference in the lives of consumers. The CardioChip™ is the heart of a powerful mHealth platform driven by complementary biometric algorithms, allowing the captured data to be instantly translated into easy-to-understand and valuable health metrics. It’s small, integrated, and is accompanied by an accessible SDK and a portfolio of biometric algorithms to lend insight into the data it collects.
For biometrics which do not require medical diagnosis or regulatory approval, CardioChip™ technology is the ideal platform for devices fulfilling consumers’ health and wellness needs.
For an immediately customizable ECG biosensor wearable, the LifeBeat™ health and fitness tracking wristband is available with proprietary NeuroSky biosensor technology—ready-to-deploy, extensible, and offering unmatched consumer value. LifeBeat™ also features an accelerometer, OLED display, vibration motor, rechargeable battery, memory, and a microcontroller within an integrated wristband form factor with flexible, comfortable rubber arms.
LifeBeat’s™ open SDK for Android and iOS platforms—along with a library of advanced fitness and health metric algorithms—enables OEM and ODM solutions providers to rapidly customize their product to showcase its abilities and help speed evaluations and time to market. The included, fully functional reference app also provides an interface to backend cloud and social media services which can be leveraged with very little time and effort.
Get In Touch With Our ECG Experts
If you have the next brilliant idea in mHealth wearable technology, you know you can’t afford to wait to bring it to market. An increasingly competitive marketplace means OEMs and ODMs need to move forward quickly while maintaining the integrity of their products.
NeuroSky has integrated ECG solutions which will help you develop innovative, behavior-changing mHealth products and bring them to market faster and better than the competition. To learn more about our integrated ECG biosensor solutions, including CardioChip™, get in touch with one of our ECG experts today.


